Managing COPD is easier with the right tools. From tracking oxygen levels to monitoring lung function, these devices empower you to stay on top of your health and avoid complications. Here's a quick look at the top devices for COPD management:
- Pulse Oximeters: Measure oxygen saturation and heart rate. Compact and affordable, starting at $15.
- Portable Spirometers: Monitor lung function (FEV1, FVC) with clinical-grade accuracy. Prices range from $99 to $2,500.
- Portable Oxygen Concentrators (POCs): Provide on-the-go oxygen therapy with FAA-approved models. Costs range from $1,000 to $3,000+.
- RESP Biosensors: Continuously track lung sounds and detect early warning signs like wheezing or coughing.
- Electronic Inhaler Monitors (EIMs): Ensure proper medication use and adherence with smart inhaler technology.
- Air Quality Monitors: Identify environmental triggers by tracking pollutants like PM2.5 and CO2. Prices start at $50.
- Fitness Trackers: Track heart rate, activity levels, and oxygen saturation with wearables like Fitbit or Apple Watch.
- Remote Patient Monitoring (RPM) Platforms: Combine multiple devices for real-time, comprehensive health tracking.
Quick Comparison:
| Device Type | Key Features | Cost Range | Best For |
|---|---|---|---|
| Pulse Oximeters | SpO₂, heart rate | $15 - $599 | Simple, daily oxygen tracking |
| Portable Spirometers | FEV1, FVC, lung function | $99 - $2,500 | Detailed lung health monitoring |
| Portable Oxygen Concentrators | Oxygen therapy on the go | $1,000 - $3,000+ | Severe oxygen needs |
| RESP Biosensors | Real-time lung sound tracking | $200 - $800 | Early detection of exacerbations |
| Electronic Inhaler Monitors | Medication adherence, reminders | $49/month | Ensuring proper inhaler use |
| Air Quality Monitors | Pollutants, temperature, humidity | $50 - $300 | Avoiding environmental COPD triggers |
| Fitness Trackers | SpO₂, heart rate, activity tracking | $100 - $499 | Encouraging physical activity |
| Remote Monitoring Platforms | Comprehensive health tracking | $100 - $500/month | Integrated COPD management with providers |
These tools help reduce hospitalizations, improve quality of life, and provide peace of mind. Choose the one that fits your lifestyle and health needs, and always consult your doctor for guidance.
The One Simple Device Every COPD Patient Must Know About - Pulse Oximetry
How to Choose COPD Monitoring Devices
Picking the right COPD monitoring device can make a big difference in managing your condition. The wrong choice could lead to inaccurate readings or frustration with overly complicated features. Here are some key factors to consider to make the process easier.
FDA Clearance and Safety Standards
Always ensure the device has FDA 510(k) clearance or Premarket Approval (PMA). This guarantees that the device meets safety and performance standards. You can confirm this by checking the FDA's 510(k) and Premarket Approvals databases or reviewing the device’s labeling and documentation. Additionally, confirm that the manufacturer is registered with the FDA for added assurance.
Accuracy and Standard Measurements
Accurate readings are essential for effective COPD management. Look for devices that measure and display data in standard units commonly used by U.S. healthcare providers. For example:
- Oxygen saturation (SpO₂): Shown as a percentage
- Flow rates: Measured in liters per minute (L/min)
- Respiratory rates: Counted in breaths per minute
Reliable measurements help detect early warning signs of a COPD flare-up.
Ease of Use for Seniors
Since many COPD patients are older adults, opt for devices with simple, intuitive designs. For example, peak flow meters, which only require a strong exhale, are often easier for home use compared to more complex spirometers. A straightforward interface can make a world of difference for those less familiar with technology.
Portability and Data Sharing
Portable devices with long battery life are ideal for monitoring on the go. Models that allow automatic data uploads to your healthcare provider ensure continuous and hassle-free tracking. This feature makes it easier to keep your care team informed without extra effort on your part.
Comfort and Wearability
Comfortable wearables, like wristbands or smartwatches, are great for long-term use. While some devices may offer precise readings, if they’re uncomfortable, you’re less likely to stick with them. Prioritize options that balance accuracy with wearability.
Support and Personal Needs
Consider your own comfort with technology, physical abilities, and age when selecting a device. Also, check that the manufacturer provides reliable technical support in case you run into any issues. Having access to help when you need it can make using the device much easier.
Studies show that remote COPD monitoring can reduce healthcare expenses by at least 14% while improving overall quality of life. Choosing a device that fits your needs and lifestyle is a vital step in staying on top of your condition.
1. Pulse Oximeters
Pulse oximeters are a key tool for monitoring COPD, offering a simple way to measure both heart rate and oxygen saturation levels in the blood. These small, clip-on devices provide vital insights into how effectively your lungs are delivering oxygen to your body. By using one regularly, you can spot drops in oxygen levels before symptoms become noticeable. For most healthy individuals, oxygen saturation levels typically range between 95% and 100%. However, levels below 90% are considered low, and readings at or below 88% may indicate a need for urgent medical attention.
Dr. Richard Castriotta, a pulmonologist and professor at the Keck School of Medicine of USC, emphasizes the importance of these devices:
"The most important tool is the pulse oximeter, and it would be best if everyone with COPD had one. These can be integrated into telemedicine visits to assess patients' status remotely in addition to aiding in self-monitoring."
Measurement Capabilities
Pulse oximeters offer quick, non-invasive measurements of SpO₂ (oxygen saturation) and pulse rate. Lower readings can indicate reduced lung or heart function, which is why regular tracking matters. Studies show that 22% of patients had oxygen saturation levels at or below 95%, while 11% recorded levels at or below 92%. These lower numbers are often linked to compromised lung function, heart conditions, and other health issues, highlighting the importance of staying vigilant.
Portability
Most at-home pulse oximeters are designed to be compact and easy to carry. Some models include handy features like carrying cases or lanyards, making them convenient for travel or daily use. Long battery life is another plus, ensuring uninterrupted monitoring. Portability is particularly valuable, as research shows that around 80% of patients feel restricted in their activities due to the limitations of their current monitoring systems.
Integration with Digital Health Platforms
Modern pulse oximeters go beyond basic functionality by integrating with digital health platforms. These advanced devices allow real-time data sharing with healthcare providers, enabling more effective management of COPD. For instance, NuvoAir Medical offers pulse oximeters that transmit data directly to clinical teams, allowing for timely interventions. Similarly, the Wellinks mHealth platform uses Bluetooth-enabled Nonin pulse oximeters to automatically log data into an app. In one study, participants - most of whom were 80 years old with severe COPD - successfully met the weekly goal of recording at least one reading. Another study using the EDGE digital health system demonstrated that pulse oximeter data, capturing oxygen saturation, pulse rate, and respiratory rate, could help predict COPD exacerbations with an accuracy score of 0.682.
These advancements in connectivity and data integration make pulse oximeters an even more powerful tool for managing COPD effectively.
2. Portable Spirometers
Portable spirometers make it possible to conduct professional lung function tests right at home, offering a practical way to monitor COPD. Unlike pulse oximeters, which measure oxygen levels, these devices focus on airflow, making them particularly helpful in tracking the breathing challenges central to COPD. This capability plays a key role in monitoring disease progression.
"Spirometry is one of the most readily available and useful tests for pulmonary function."
Measurement Capabilities
These devices provide detailed insights into lung function by measuring parameters like FEV1 (forced expiratory volume in one second), FVC (forced vital capacity), the FEV1/FVC ratio, and peak expiratory flow (PEF). These metrics help identify airflow restrictions and support early intervention when needed.
Studies show that portable spirometers are highly accurate for diagnosing COPD, with a sensitivity and specificity of 0.85 each. The area under the curve (AUC) stands at 0.91, indicating strong diagnostic reliability. Devices capable of measuring multiple indices tend to deliver even better accuracy.
Portability
Today’s portable spirometers, like the SpiroSonic AIR and MIR Spirobank II Basic, are designed for convenience. They’re lightweight, compact, and offer long battery life, making them ideal for daily use and travel.
| Device | Weight | Dimensions | Battery Life | Key Features |
|---|---|---|---|---|
| SpiroSonic AIR | 142g | 45 × 73 × 95 mm | 10+ hours | Wireless charging, Bluetooth 4.0 |
| MIR Spirobank II Basic | 140g | 160 × 55 × 25 mm | 40 hours | High-resolution display, large memory |
| CMI Health SpiroLink | Not specified | Compact design | 6 days active / 30 days idle | Bluetooth Low Energy, cloud app |
| MIR Spirolab | 1,450g | 220 × 210 × 51 mm | 10 hours | Touchscreen, optional oximetry |
Integration with Digital Health Platforms
Connectivity is a game-changer in COPD management. By linking portable spirometers with digital health platforms, patients and healthcare providers can monitor trends in lung function, symptoms, and activity levels. This approach has been shown to reduce hospital admissions by 35% while enhancing telemedicine capabilities.
The growing role of digital health is reflected in the mHealth apps market, which was valued at $38.2 billion in 2021 and is projected to grow 11.8% annually through 2030. This trend highlights the increasing importance of integrating portable spirometers with mobile apps and other digital tools.
Cost
Portable spirometers are a budget-friendly alternative to traditional lab equipment. They enable early detection and reduce hospital visits, which can significantly cut healthcare costs. By delivering clinical-grade accuracy at a much lower price point, these devices provide an effective way to manage COPD proactively.
3. Portable Oxygen Concentrators
Portable oxygen concentrators (POCs) play a crucial role in helping patients with COPD take charge of their condition. These devices work by purifying ambient air to deliver oxygen concentrations of 90%-95%, eliminating the inconvenience of refilling tanks. When connected to a power source, they provide a steady, unlimited oxygen supply. Today, more than 1.5 million Americans rely on POCs for supplemental oxygen therapy. Their convenience and efficiency make them a valuable addition to COPD management routines.
Portability
One of the standout features of POCs is their portability. Unlike stationary concentrators, which can weigh around 22 pounds and require a constant electrical connection, POCs are much smaller and lighter. Many models are also FAA-approved, allowing patients to travel on commercial airlines without hassle.
Battery life varies by model. Single-battery units typically last between 2 and 6 hours, while double-battery models can extend usage to 5–13 hours. On average, patients use their POCs for about 4.3 hours daily, recharging the batteries intermittently as needed.
Integration with Digital Health Platforms
POCs are not just portable - they’re also designed for ease of use. Many modern models feature straightforward controls, clear displays, and options for both pulse-flow and continuous flow oxygen delivery, allowing patients to customize their therapy. For instance, the Inogen One System is built for continuous use, whether at home, in care facilities, or on the move, making it an excellent choice for those who need consistent oxygen support.
Cost
The cost of POCs can vary widely. New devices typically range from $1,500 to $4,000, while used units are available for $800 to $2,500. Rental options provide additional flexibility, with daily rates around $35 and weekly rates between $85 and $450, depending on the model and terms. Beyond the initial purchase or rental cost, patients should factor in ongoing expenses like electricity for recharging, maintenance, and replacement batteries. For example, the Belluscura X-Plor is priced at approximately $2,000 for the base unit and $2,500 for a travel package. While the upfront investment can be significant, the benefits - such as improved sleep, mood, and daily activity levels - make these devices a valuable tool for effective COPD management.
4. RESP Biosensor
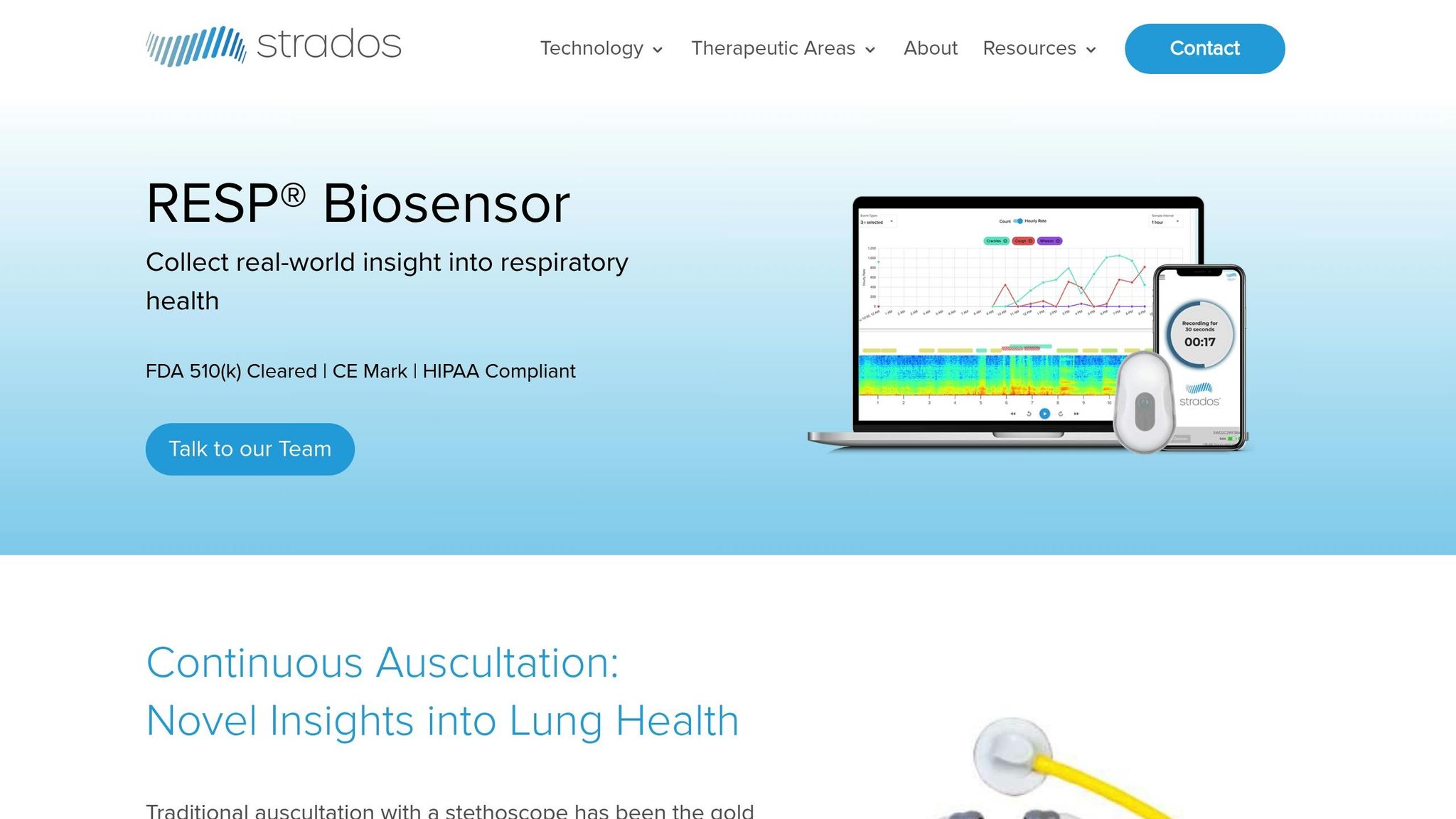
The RESP Biosensor transforms how COPD patients are monitored by providing continuous respiratory data. Acting like a 24-hour digital stethoscope, the device captures lung sounds in real time, tracking early warning signs like coughing and wheezing. Unlike traditional methods that rely on scheduled check-ups, this biosensor delivers constant updates, helping predict flare-ups before they escalate into serious complications.
"This data enables early intervention to prevent complications." - Sadia Benzaquen, MD, Chair of Pulmonary Critical Care, Einstein Medical Center
This kind of proactive monitoring is crucial, especially since one in five COPD patients is readmitted to the hospital within just a month of discharge. Studies reveal that increased coughing can signal exacerbations up to 3.4 days in advance, giving healthcare teams a vital window to act.
Measurement Capabilities
The RESP Biosensor doesn’t just monitor - it provides a comprehensive look at respiratory health. By continuously recording pulmonary sounds for 24 hours, the device tracks:
- Cough frequency and severity
- Cough type (dry or productive)
- Other respiratory events, such as wheezing, rhonchi, and crackles
This data is time-stamped and highly accurate, offering healthcare providers a clearer picture of a patient’s condition and how they’re responding to treatment. The lung sound recordings are presented as spectrograms, making it easier for clinicians to spot patterns and changes. For instance, in one case, a patient exhibited a 44% increase in cough and a 119% rise in wheezing between days 3 and 4 post-discharge. Five days later, the patient was readmitted. This highlights how the RESP Biosensor can catch warning signs that might otherwise go unnoticed.
Portability
Designed with comfort and convenience in mind, the RESP Biosensor is lightweight and easy to wear daily. Weighing just 3.5 ounces (100g), it measures 3.3" x 2" x 0.39" - about the height and width of a credit card and the depth of a mobile phone.
Its 24+ hour battery life ensures uninterrupted use, and the device is both rechargeable and reusable, making it a practical choice for long-term care. Patients often report that they forget they’re even wearing it, as it’s designed to seamlessly integrate into daily life without causing disruptions.
Integration with Digital Health Platforms
The RESP Biosensor goes beyond just collecting data - it integrates smoothly with existing healthcare systems. It’s compatible with EHR and telehealth platforms and complies with HIPAA standards to ensure patient data remains secure.
Here’s how the system works: the device captures lung sounds and respiratory rates, then transmits the data via Bluetooth to a mobile app. From there, the information is sent to the Strados cloud through Wi-Fi or cellular networks. Healthcare providers can access this data remotely, enabling around-the-clock monitoring without requiring patients to visit the clinic.
The biosensor also employs proprietary machine learning algorithms to automatically detect events like coughs and wheezes. This technology supports the remote management of respiratory conditions such as COPD and asthma, empowering healthcare teams to intervene early and prevent minor issues from escalating.
Cost
While the exact price of the RESP Biosensor isn’t publicly disclosed, it’s typically prescribed as part of a broader COPD management plan. Many patients receive the device during high-risk periods, such as the two weeks following hospital discharge.
The potential cost savings are substantial. With COPD readmission rates exceeding 20% within 30 days, early intervention through the RESP Biosensor can significantly reduce hospitalizations and overall healthcare expenses. If you’re considering this device, speak with your healthcare provider about coverage options and how it fits into your care plan.
5. Electronic Inhaler Monitors
Electronic inhaler monitors (EIMs) turn traditional inhalers into smart devices by incorporating digital sensors and smartphone connectivity to track each dose taken. This technology plays a key role in managing COPD (chronic obstructive pulmonary disease), where long-term maintenance therapy adherence is often alarmingly low - averaging just 50% or less. This lack of adherence not only impacts patient health but also comes with a hefty price tag, costing the U.S. healthcare system between $100 billion and $290 billion annually.
Measurement Capabilities
EIMs use advanced sensors to record the exact time and date of each inhaler actuation. Some models go a step further, measuring inhalation airflow and ensuring proper use of pressurized metered-dose inhalers. These devices can track missed controller doses, detect overuse of rescue medications, and evaluate inhalation techniques. By combining this data with symptom tracking, environmental conditions, and physiological metrics, EIMs enable more tailored COPD management strategies.
Data from EIMs can also support healthcare providers in improving outcomes. For example, studies have shown that active monitoring by clinicians using EIM data increased adherence rates by 18% compared to passive monitoring. Additionally, 85% of users found the digital platforms easy to use, and 91% appreciated the inhaler reminders.
Portability
EIM sensors attach directly to inhalers or come pre-installed within the device, adding little extra bulk. They connect to smartphones via Bluetooth and offer a battery life that lasts through multiple inhaler refills. Their lightweight design ensures they feel just as convenient as standard inhalers.
Integration with Digital Health Platforms
Each EIM pairs with a dedicated mobile app that collects data and interacts with users. These apps provide reminders for controller medications, track environmental triggers, and display usage trends. Some apps even integrate location data with environmental reports to help identify potential triggers. By syncing with internet-connected smartphones, the data becomes accessible to clinicians - if users consent - allowing real-time monitoring of adherence, inhaler technique, and medication use.
This data integration doesn’t stop at the app. Information from EIMs can be linked to electronic health records, enabling prescribers to incorporate it into a patient’s medical history. This connectivity helps refine treatment plans and can contribute to more effective, cost-efficient care.
Cost
The cost of electronic inhaler monitors depends on the device and insurance coverage. A standard albuterol inhaler ranges from $5 to $60, while digital sensors like the Propeller system were priced at around $300 as of 2017. Insurance coverage varies by device, but some prescription-only options, like CapMedic, may be covered and billed directly through medical insurance, potentially reducing out-of-pocket expenses.
As insurers increasingly recognize the benefits of these devices in reducing healthcare costs, coverage is expected to grow. By improving adherence, EIMs can lead to fewer emergency room visits and hospitalizations, ultimately saving money for both patients and the healthcare system. While the upfront cost may seem high, the long-term savings and improved health outcomes make these devices a worthwhile investment.
sbb-itb-3e96dba
6. Air Quality Monitors
Air quality monitors play a crucial role in managing COPD by acting as early warning systems for environmental triggers. Since indoor air can contain 2 to 5 times more pollutants than outdoor air, these devices are particularly important for monitoring the home environment, where many COPD patients spend the majority of their time. This integration of environmental data with health platforms reflects the growing emphasis on personalized COPD management tools.
"Indoor air quality is critical to everyone's health, especially people living with chronic obstructive pulmonary disease (COPD)." - Editorial Staff, American Lung Association
Measurement Capabilities
Today's air quality monitors can track a wide range of pollutants that directly affect COPD symptoms. These include particulate matter (PM2.5 and PM10), nitrogen dioxide (NO2), carbon monoxide (CO), and ozone (O3). Many models also measure temperature, humidity, CO2, and radon levels. For example, exposure to nitrogen dioxide can increase the risk of a COPD exacerbation by 33% with each interquartile range increase. Indoor particles are also known to reduce peak expiratory flow (PEF). These pollutants contribute to lung inflammation, worsening symptoms, and reducing overall lung function.
Portability
Portable air quality monitors are designed to be lightweight and convenient. The QP Lite, for instance, weighs just 0.31 lbs (143 g) and offers a battery life of 4–6 hours, making it easy to use both indoors and outdoors. For those needing more advanced monitoring, the Aeroqual Ranger weighs under 15 oz (430 g) and boasts a battery life of over 20 hours. These compact devices enable COPD patients to test air quality in various locations - whether at home, work, or outdoors - before spending extended time there. Their small size allows them to fit easily into a purse or backpack, making on-the-go monitoring simple.
Integration with Digital Health Platforms
When paired with digital health platforms and smartphone apps, air quality monitors become even more effective for COPD management. For example, the QP Lite connects to the Qingping+ app, enabling remote monitoring and data export for further analysis. Advanced models like the Aeroqual Ranger support Wi-Fi and USB data transfer. A notable example of such integration is the AIR Louisville program (2015–2016), which combined air quality data with smart inhaler sensors. Over 12 months, the program collected 1.2 million data points, including over 251,000 medication puffs and 5.4 million environmental data points like air pollutants, temperature, and traffic proximity. The results were striking: participants saw an 82% drop in rescue inhaler use, 29% of previously uncontrolled participants gained control of their asthma, symptom-free days more than doubled, and symptom-free nights increased by 19% on average.
Cost
Air quality monitors come in a wide price range, depending on their features and capabilities. The QP Lite, for instance, is priced at $99 as of April 2025, offering basic monitoring for particulate matter, CO2, temperature, and humidity. On the higher end, professional-grade devices like the Aeroqual Series 500 provide measurements for up to 30 different pollutants but come at a much steeper cost. For those on a budget, options like the Qxpztk 10-in-1 Indoor Air Quality Monitor are available, though reviews are mixed. This model holds a 4.2/5 star rating from 31 users on Amazon, with praise for its ease of use and clear display, but some concerns about accuracy and battery life. For COPD patients, investing in a reliable and accurate monitor is essential, as the data directly influences health decisions and symptom management.
7. Fitness Trackers with Health Monitoring
Fitness trackers have become a valuable tool for managing COPD, offering continuous monitoring of vital signs and activity levels. These wearables can detect subtle changes that might signal a worsening of symptoms, complementing data from clinical devices to provide a more complete picture of a patient’s health.
A study conducted by McGill University Health Centre followed 21 COPD patients over 21 days and found that recovery was linked to improvements in heart rate, respiratory rate, oxygen saturation, and sleep quality. On the other hand, persistent symptoms were associated with ongoing abnormalities in these metrics, poor sleep efficiency, and reduced activity levels.
"Wearable technology gives us unprecedented insights into how the lungs, heart, and nervous system respond during COPD exacerbations. This knowledge can lead to earlier interventions and better outcomes." – Dr. Bryan Ross, Study Lead
Measurement Capabilities
Modern fitness trackers are equipped to measure a wide range of health metrics. Devices like the Amazfit Band 7 and Apple Watch Series 6 can track heart rate, blood oxygen levels (SpO₂), stress, and sleep quality. They also offer alerts when vital signs fall outside normal ranges, helping users stay proactive about their health.
SpO₂ monitoring is particularly important for COPD patients. A 2023 study found a moderate correlation between smartwatch SpO₂ readings and traditional blood gas measurements (ICC: 0.502, p: 0.004). However, accuracy may decrease during respiratory distress. For example, the Apple Watch Series 6 uses reflectance pulse oximetry, which can be affected by ambient light. Additionally, the Apple Watch combines sleep tracking with nocturnal oximetry, which can aid in identifying sleep apnea - a common condition among COPD patients.
Portability
Fitness trackers are designed to be lightweight and convenient. For instance, the Fitbit Inspire 3 weighs just 0.32 ounces and boasts a 10-day battery life, while the Garmin Forerunner 265S weighs 39 grams and lasts up to 13 days. Battery life varies widely depending on the model, with some like the Garmin Instinct 2X Solar offering up to 40 days in smartwatch mode - or even unlimited battery life under sufficient solar exposure. Similarly, the Withings ScanWatch 2 provides up to 30 days of use, whereas the Apple Watch SE (2nd generation) requires daily charging with its 18-hour battery life.
Integration with Digital Health Platforms
Fitness trackers integrated with digital health platforms and AI analytics are changing the way COPD is managed. Unlike stationary monitoring devices, wearables capture health data during everyday activities, offering insights into patterns that might otherwise go unnoticed. AI and machine learning tools can analyze this data to predict health outcomes and support personalized care plans.
Studies show that wearable technology can encourage more physical activity. A meta-analysis revealed that fitness trackers increased users’ daily step count by an average of 850 steps and improved their six-minute walk distance by 5.81 meters. When combined with health coaching or pulmonary rehabilitation, these benefits become even more pronounced. By detecting symptoms early, wearables could also help reduce hospitalizations - a critical advantage given that COPD ranks as the third leading cause of hospital readmissions in the U.S. as of 2023.
Cost
Fitness trackers are available at a wide range of price points, from $99.99 to $449.99, making them a practical addition to COPD care. Budget-friendly options like the Fitbit Inspire 3, priced at $99.99, were highlighted by Wirecutter in May 2025 as the most accurate for step tracking. The Fitbit Charge 6, retailing at $159.99, offers additional features and holds a 4.0/5 rating on Best Buy. Mid-range options include the Amazfit Balance at $229.99, which boasts a 14-day battery life. Premium models like the Withings ScanWatch 2 ($349.99) and the Garmin Instinct 2X Solar ($449.99) provide advanced health tracking and extended battery life, with the Garmin Forerunner 265S also priced at $449.99.
8. Remote Patient Monitoring Platforms
Remote patient monitoring (RPM) platforms bring together multiple FDA-cleared devices to provide real-time health data, enabling early medical intervention. This coordinated system lays the groundwork for the detailed monitoring capabilities outlined below.
A study conducted by Pulmonary Associates of Richmond and Spire Health highlights the impact of RPM on managing COPD. Among 126 patients who used COPD-focused remote monitoring for at least a year, the results were striking: a 65% drop in all-cause hospitalizations, a 63.6% reduction in cardiopulmonary hospitalizations, and a 44.3% decrease in emergency room visits. Notably, patient engagement remained high, with 88.6% of days meeting the 8-hour daily wear requirement.
Measurement Capabilities
RPM platforms track a variety of health metrics, including lung capacity, SpO₂, pulse, blood pressure, temperature, and FEV1, helping to predict potential exacerbations.
These platforms also incorporate advanced tools for respiratory monitoring. Devices like peak flow meters and oscillometers assess lung function, while wearable accelerometers and chest bands provide precise respiratory rate measurements. A UCLA study found moderate correlations between reduced FEV1 levels and self-reported healthcare events, as well as between SpO₂ readings below 90% and exacerbations.
In addition to respiratory data, RPM systems monitor activity levels and sleep patterns to maintain ongoing patient engagement. Efficient data transfer further enhances these capabilities, ensuring healthcare providers can act quickly when needed.
Integration with Digital Health Platforms
Building on earlier monitoring tools, modern RPM platforms centralize patient data, enabling timely and informed clinical decisions. They integrate seamlessly with electronic health records (EHRs) using FHIR and HL7 standards, reducing manual data entry errors. With more than 85% of U.S. hospitals now using EHRs, this integration is essential for widespread adoption.
RPM systems convert real-time data into actionable insights, supporting prompt medical interventions. Research shows that integrating RPM with EHRs can reduce hospital readmissions by up to 38% and improve chronic disease management outcomes by 25%.
Frederick Memorial Hospital’s Chronic Care Management Program serves as a strong example of successful RPM integration. By using a system that bidirectionally synced with their EMR, Healthwyse, they saw an 89% drop in hospital readmissions, a 49% reduction in emergency department visits, and a 52% decrease in average care costs for enrolled patients.
"EMR integration is crucial to an effective RPM program on multiple levels. Patient care is more efficient by allowing RPM data to be viewed within the EMR for seamless record review documentation, and orders." – Dr. David Voellinger of Novant Health Bariatric Solutions
Cost
While RPM platforms are more expensive than standalone devices, they often lead to significant overall savings in healthcare costs. On average, RPM costs range from $100 to $500 per patient per month, with annual expenses typically between $1,000 and $2,000 per patient.
The cost of RPM varies based on several factors, including the type of monitoring needed, data collection frequency, device sophistication, software features, and support services. Billing for RPM services is covered under HCPCS codes, such as 98975 ($19.38), 98976 ($55.72), and 98980 ($50.18).
Support for RPM technology is growing, with around 80% of patients expressing approval. Key reasons for adoption include convenience (43%), improved care efficiency (39%), better health control (37%), enhanced diagnostic accuracy (36%), and peace of mind (36%). By 2025, approximately 26.2% of the U.S. population is expected to benefit from remote patient monitoring. Despite the upfront costs, the reductions in hospitalizations and emergency visits make RPM a valuable investment in patient care.
Device Comparison Table
Choosing the right device for managing COPD can feel overwhelming, but this comparison table breaks down the options to help you find one that suits your lifestyle, needs, and budget.
| Device Type | Measurement Capabilities | Portability | Digital Platform Compatibility | Cost Range | Key Advantages | Main Disadvantages |
|---|---|---|---|---|---|---|
| Pulse Oximeters | SpO₂, heart rate | Extremely portable (finger/wrist-worn) | Limited standalone integration | $15 - $599 | Quick readings, affordable, simple to use | Can be inaccurate; minimal data storage |
| Portable Spirometers | Lung volume, airflow (FEV1) | Compact and travel-friendly | Moderate smartphone connectivity | $99 - $2,500 | Detailed lung function analysis | Requires effort from the user; testing can be tiring |
| Portable Oxygen Concentrators | Oxygen delivery (LPM), pulse dose settings | Designed for mobility (3.3–4.6 kg on average) | Basic monitoring integration | $1,000 - $3,000+ | Offers continuous or pulse oxygen; travel-approved | Heavier for extended use; battery life may be limiting |
| RESP Biosensors | Lung sounds, coughing, wheezing patterns | Wearable, chest-mounted | Advanced smartphone/tablet pairing | $200 - $800 | Tracks respiratory sounds in real time | Limited availability; needs precise placement |
| Electronic Inhaler Monitors | Medication usage, adherence, technique | Clips onto existing inhalers | Excellent app integration | $49/month (Cohero Health) | Monitors medication use and provides feedback on technique | Subscription costs; potential compatibility issues |
| Air Quality Monitors | Environmental pollutants, particulates | Available in portable and stationary models | Smart home integration | $50 - $300 | Helps identify environmental triggers | Does not track body functions directly |
| Fitness Trackers with Health Monitoring | Heart rate, activity levels, sleep patterns | Lightweight, wrist-worn | Excellent smartphone/health app sync | $100 - $499 (Omron HeartGuide) | Continuous activity tracking; promotes healthier habits | Limited respiratory-specific data |
| Remote Patient Monitoring Platforms | Multi-device integration (SpO₂, FEV1, BP, temp) | Varies depending on devices used | Full EHR integration via FHIR/HL7 standards | $100 - $500/month per patient | Comprehensive tracking; integrates with clinical systems | Higher cost; may need professional setup assistance |
Key Considerations for COPD Device Selection
For budget-conscious users, devices like pulse oximeters or air quality monitors provide basic yet useful insights, with prices starting as low as $15. On the other hand, premium devices such as portable spirometers or remote patient monitoring platforms offer more extensive tracking and advanced features, but they come with higher price tags.
Wearable devices, like RESP biosensors or fitness trackers, are particularly appealing for long-term use due to their comfort and convenience. If your goal is professional healthcare integration, platforms that sync with EHR systems using FHIR/HL7 standards ensure seamless communication with your care team.
When choosing a device, think about your specific needs - whether it’s portability, ease of use, or advanced monitoring capabilities - and how much integration with healthcare providers or personal tracking you require. By focusing on these priorities, you can find the device that aligns best with your COPD management goals.
How to Use and Maintain Your Devices
Taking care of COPD devices is essential to ensure they work accurately and last longer. Each device has its own maintenance needs, so knowing how to clean, store, and calibrate them properly is key.
Cleaning Your Devices Safely
For pulse oximeters, always switch off the device and unplug it before cleaning. Use a soft cloth dampened with a mild detergent solution to wipe the surfaces. Then, disinfect it with a 70% isopropyl alcohol solution, focusing on the silicone finger contact area. For hard-to-reach spots like sensors and buttons, a cotton swab works well. Let the device air dry completely before using it again.
Spirometers need more detailed cleaning because they come into contact with respiratory secretions. Use a fresh bacterial viral filter for each test. After every use, wipe the outer surfaces and flowhead with a 70% isopropyl alcohol cloth. For a deeper clean, disassemble the turbine and mouthpiece. Prepare a cleaning solution by mixing ¾ cup of Clorox™ bleach (7.5%) with one quart of water. Soak the turbine for one minute, let it sit for 15 minutes, and shake the mouthpiece in the solution for 2–3 minutes. Rinse both parts thoroughly with clean water, shake off excess water, and dry them with paper towels. Proper storage after cleaning is equally important to maintain the device's functionality.
Storage Best Practices
Store your pulse oximeter in a dry, dust-free area, and if you won’t use it for a while, remove the batteries. For spirometers, make sure all parts are completely dry before storing, and follow the manufacturer's instructions. Portable oxygen concentrators should be kept in a clean, temperature-controlled space. Check the owner's manual for specific temperature guidelines, as both extreme heat and cold can impact performance.
Calibration and Professional Maintenance
While most consumer devices don’t need frequent calibration, professional-grade equipment often does. Follow the service schedule recommended by the manufacturer. For example, portable oxygen concentrators typically need annual maintenance. Always rely on certified technicians for calibration to ensure accuracy.
Interpreting Your Readings
Knowing what your device readings mean can help you decide when to seek medical help. For pulse oximeters, normal oxygen saturation levels are usually between 95% and 100%, though your healthcare provider may set a different target range for you. Spirometry results, like the forced expiratory volume in 1 second (FEV1), provide a snapshot of lung function. Research shows that quitting smoking can significantly slow the decline of FEV1 - by about 31 mL per year compared to 62 mL per year in those who continue smoking. Understanding these readings and spotting changes early can lead to quicker medical intervention.
Recognizing Warning Signs
Be alert for symptoms such as shortness of breath, a persistent cough with sputum, wheezing, chest tightness, or unusual fatigue. If your device consistently shows abnormal readings or you notice a downward trend, contact your healthcare provider right away. Changes in breathing patterns or activity levels should also be discussed with your doctor, as early action can help prevent complications.
| Device Type | Cleaning Frequency | Storage Requirements | Professional Maintenance |
|---|---|---|---|
| Pulse Oximeter | After each use; deep clean as needed | Dry, dust-free area; remove batteries for long-term storage | Periodic calibration as recommended |
| Spirometer | Wipe after each use; deep clean per guidelines | Ensure all parts are dry; follow manufacturer instructions | Annual professional servicing required |
| Oxygen Concentrator | Clean exterior; follow manual for filter changes | Temperature-controlled, clean environment | Annual service and filter replacement |
Troubleshooting Common Issues
If your pulse oximeter shows inconsistent results, check for common issues like nail polish, cold fingers, or movement during testing. Warm your hands and ensure your finger is clean and dry before using the device. For spirometers, improper technique is a frequent cause of errors. Make sure to take a full breath, seal your lips tightly around the mouthpiece, and exhale forcefully. If your oxygen concentrator makes unusual noises or airflow is reduced, the filters may be clogged. Refer to the user manual for instructions on replacing or cleaning the filters.
Conclusion
COPD monitoring devices, ranging from pulse oximeters to electronic inhaler monitors, provide a clear and detailed picture of your respiratory health.
Research involving 126 COPD patients using remote monitoring showed impressive results: a 65% reduction in all-cause hospitalizations, 63.6% fewer cardiopulmonary events, and a 44.3% decrease in ER visits, with patients adhering to their monitoring routines 88.6% of the time.
"By integrating RPM into COPD management, healthcare organizations can empower patients and providers with the tools and knowledge to proactively manage their condition while enhancing health outcomes and quality of life."
These devices play a critical role in identifying symptoms early, often before they escalate into serious issues. Remote monitoring bridges the gap between the onset of flare-up symptoms and clinical intervention, which can significantly reduce the likelihood of hospitalizations. The evidence highlights how early detection and timely action can lead to better outcomes. Given the impact of COPD, monitoring is an essential component of effective care.
Consistency is key. Using these devices daily and maintaining open communication with your healthcare provider ensures that the data they collect can guide necessary adjustments to your treatment plan.
Incorporate these tools into your routine alongside regular check-ins with your doctor. With proper use and maintenance, these devices can help you manage your condition more effectively and improve your overall quality of life.
FAQs
Choosing the right COPD monitoring device hinges on your specific health needs and the stage of your condition. Spirometers are great for keeping tabs on lung function and tracking how the disease progresses over time. On the other hand, pulse oximeters are widely used to measure oxygen levels, which is especially helpful if you rely on supplemental oxygen. For those seeking more comprehensive monitoring, wearable devices can continuously track your breathing patterns, offering a convenient way to manage symptoms from home.
When deciding which device suits you best, think about your daily routine, lifestyle, and medical needs. And remember, discussing your options with a healthcare provider is key - they can guide you toward the devices that will help you manage your symptoms most effectively.
Portable oxygen concentrators (POCs) are a valuable tool for many people managing COPD, but they come with a few limitations. For instance, flow rates on these devices typically range from 1 to 5 liters per minute. While this is sufficient for many, it may not meet the higher oxygen demands of individuals dealing with severe symptoms, particularly during physical activity or flare-ups.
Another consideration is that POCs depend on electrical power to operate. This means they won’t work during power outages unless you’ve arranged for a backup power source.
Some users have also expressed concerns about the reliability and performance of POCs, which can affect their confidence in using them to manage symptoms effectively. For these reasons, it’s essential to discuss your needs and lifestyle with your healthcare provider to determine whether a POC is the right choice for you.
Combining digital health tools with COPD devices can transform the way you manage your condition. These tools enable real-time symptom tracking and provide tailored feedback, helping you spot early warning signs of flare-ups. Catching these signs early means you can act faster, which can lead to better control over your symptoms.
Devices like smart inhalers and sensors also play a key role in improving medication adherence and ensuring proper inhaler technique - both critical aspects of managing COPD. By incorporating these technologies into your care routine, you can take charge of your health, potentially cut down on hospital visits, and work toward a better day-to-day quality of life.









