COPD exacerbations can escalate quickly and lead to severe complications if not addressed promptly. Recognizing the early warning signs is crucial to managing your condition and avoiding hospital visits. Here's what you need to know:
- What is a COPD Exacerbation? A sudden worsening of symptoms like increased shortness of breath, coughing, or mucus production beyond your usual baseline.
- Common Triggers: Respiratory infections (viruses, bacteria), smoke, air pollution, allergens, and weather changes.
- Early Warning Signs: Persistent or worsening shortness of breath, changes in mucus color or consistency, and increased fatigue.
- Emergency Symptoms: Severe breathlessness, confusion, blue lips or nails, chest pain, or oxygen levels below 88%. Call 911 immediately if these occur.
- Tools for Monitoring: Devices like pulse oximeters, peak flow meters, and symptom tracking apps can help you catch changes early and act quickly.
- Prevention Tips: Avoid triggers like smoke and poor air quality, stick to your treatment plan, and stay consistent with medications and vaccinations.
Act fast when symptoms worsen. Use your COPD action plan, monitor your condition, and consult your healthcare provider when needed. Early detection and proactive management can protect your lung health and quality of life.
What Are COPD Exacerbations
Definition of a COPD Exacerbation
A COPD exacerbation happens when your respiratory symptoms - like coughing, increased mucus, or shortness of breath - worsen beyond what’s typical for you. This isn’t just a minor fluctuation; it’s a noticeable decline in your condition. Identifying these episodes is critical since nearly half of all acute exacerbations go unreported, which can lead to serious long-term effects.
"Most patients find it difficult to identify the very early stages of an exacerbation and to distinguish their worsening symptoms from day-to-day variability." - Jing Zhang et al., Department of Pulmonary and Critical Care Medicine, Peking University Third Hospital [3]
If left untreated, an exacerbation can cause permanent lung damage, making everyday tasks - like walking short distances or climbing stairs - much harder over time.
Common Triggers That Cause Exacerbations
Respiratory infections are the most common triggers, with viruses responsible for about half of all cases. Among these, human rhinoviruses - the cause of the common cold - are the most frequent offenders [2]. Bacterial infections are another major factor, with studies showing an increase in bacterial colonization from 48.2% in stable COPD patients to 69.6% during an exacerbation [2].
Environmental factors also play a big role. Air pollution is linked to higher hospitalizations for COPD, and exposure to smoke - whether from cigarettes, secondhand smoke, wood-burning fires, or campfires - can increase your risk [2]. Weather extremes, like cold, windy days or hot, humid conditions, can irritate your airways and make breathing harder. Additionally, chemical irritants from cleaning products, strong perfumes, and aerosol sprays, along with allergens like dust mites, pet dander, and pollen, can aggravate symptoms or trigger flare-ups.
Understanding these triggers highlights the importance of paying attention to your usual symptom patterns.
Know Your Normal Symptoms
Once you’re aware of potential triggers, it’s equally important to recognize what’s “normal” for you. Everyone with COPD has their own baseline - whether that’s a mild morning cough, slight shortness of breath during daily activities, or a small amount of clear mucus. The key is noticing when these symptoms worsen or change. For example, a persistent cough or changes in mucus color or consistency could be early warning signs.
Episode 09 : Exacerbations or Worsening COPD. Which is it?
Early Warning Signs to Watch For
It's crucial to recognize when your respiratory symptoms worsen and persist for two or more days, as this can help you avoid serious complications. These changes often go beyond your usual symptoms, becoming more intense and progressively worse [5]. Knowing when your typical COPD symptoms escalate into something more concerning is the first step. Let’s dive into the physical and emergency signs you should keep an eye on.
Physical Symptoms That Signal Problems
One of the clearest indicators of a potential exacerbation is when your respiratory symptoms significantly worsen [4]. Keeping track of your baseline symptoms can help you notice changes, such as increased shortness of breath or needing more effort to breathe.
Breathing difficulties often appear first. You might find yourself getting out of breath during activities that were previously manageable, or even while at rest. If your breathing feels more labored than usual, it could mean your body is struggling to get enough oxygen.
Emergency Symptoms That Need Immediate Care
Certain symptoms are red flags that require urgent medical attention. These signs point to a critical decline in your condition and should not be ignored.
- Call 911 immediately if you experience severe breathing problems, such as breathlessness while at rest, trouble speaking, or shortness of breath that disrupts your daily activities [8–14]. If your rescue medications fail to provide relief, seek emergency help right away [11–12].
- Changes in mental state, like confusion, disorientation, slurred speech, extreme fatigue, or difficulty staying awake, may signal that your brain isn't getting enough oxygen [8–14].
Other serious warning signs include:
- Skin discoloration: A blue or gray tint to your skin, lips, or nails, which indicates low oxygen levels [8–14].
- Chest pain or tightness: Especially if the pain radiates to your arms, back, neck, or jaw [8–14].
- High fever: Particularly if it’s accompanied by shaking chills [6][7][8][10].
- Heart rate issues: Rapid breathing or a racing heartbeat [6][7][9][10].
- Coughing up blood: This symptom always requires immediate medical attention [6][8][9].
These symptoms are your body's way of signaling that it needs help. Acting quickly can make a significant difference in managing your condition.
Tools and Methods for Tracking Symptoms
Keeping a close eye on symptoms is essential for managing COPD effectively. By using the right tools, you can detect subtle changes early and take action before symptoms worsen. Here’s a look at some of the most useful tools for monitoring your condition.
Devices for Early Detection
Pulse oximeters are indispensable for monitoring blood oxygen levels. These devices can alert you to drops in oxygen saturation before you experience severe shortness of breath. While normal oxygen levels range between 95% and 100%, individuals with COPD often see baseline levels between 88% and 92%. A drop of 4% or more from your typical range is a sign to contact your healthcare provider.
Peak flow meters offer a straightforward way to measure how quickly you can exhale. This helps you track changes in your breathing capacity over time. These portable devices, priced between $15 and $30, are easy to use and provide valuable insights when used consistently, especially in the morning when your baseline is most stable.
Symptom tracking tools, like digital apps or written journals, allow you to log details such as energy levels, cough patterns, sputum changes, and sleep quality. By tracking these factors daily for 2–3 weeks, you can uncover patterns that might otherwise go unnoticed.
Smart thermometers are another handy tool, helping you monitor for fevers that often signal respiratory infections. These devices store temperature history, making it easier to identify trends and share data with your doctor.
Resources from COPD Essentials
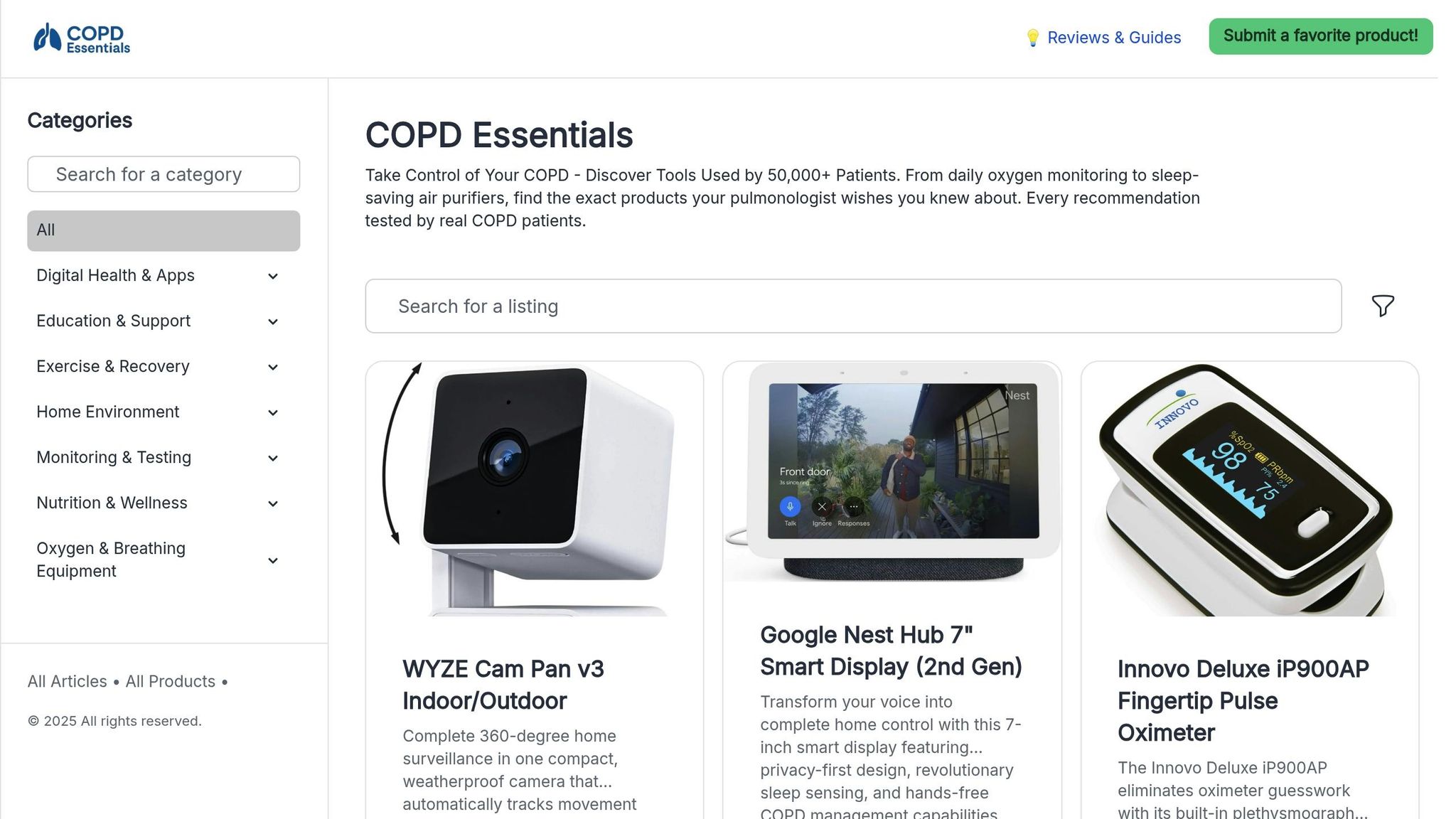
For those seeking a comprehensive approach, COPD Essentials offers a range of tools tailored specifically to COPD management. Their collection includes:
- Pulse oximeters for both daily checks and overnight monitoring, which help detect oxygen level drops during sleep - a time when changes can easily go unnoticed.
- Home spirometers, which provide more detailed lung function data than peak flow meters. These devices can identify subtle declines in breathing capacity, enabling you and your doctor to adjust treatments proactively.
- Air quality monitors to track indoor triggers like particulate matter and humidity. Pairing these monitors with HEPA air purifiers can help you both identify and reduce environmental irritants in your home.
- Symptom tracking tools, available as apps or physical journals, designed to focus on the key metrics that matter most for early detection of exacerbations.
- Connected devices that sync directly to your smartphone, simplifying record-keeping and ensuring you stay on top of any changes in your condition.
Each tool offered by COPD Essentials has been carefully reviewed by health researchers, so you can feel confident in their reliability and effectiveness. These resources work together to help you stay ahead of potential issues and manage your symptoms with precision.
sbb-itb-3e96dba
Steps to Take When Symptoms Get Worse
When symptoms of COPD worsen, quick action can help you avoid serious complications. Having a clear plan in place and knowing when to seek help can make managing your condition much easier.
Use Your COPD Action Plan
Your COPD action plan is your guide when symptoms change. This plan, created with your healthcare provider, outlines specific steps tailored to your condition and medications. If you don’t already have one, ask your doctor to help you create one at your next visit.
At the first signs of worsening symptoms - like increased shortness of breath, chest tightness, or wheezing - use your rescue inhaler (2–4 puffs) right away. Most plans recommend short-acting bronchodilators like albuterol. Wait 15–20 minutes to see if your symptoms improve. If they don’t, a second dose may be needed.
While waiting for the medication to take effect, sit upright and lean slightly forward to make breathing easier. This position helps open your airways and reduces the effort needed to breathe.
Keep an eye on your oxygen levels before and after using your inhaler. A drop of more than 4% or levels falling below 88% can signal that your symptoms are worsening and may require further action.
Stick to the medication adjustments outlined in your action plan. Avoid making any changes to your medication doses without consulting your doctor. Monitor your symptoms closely over the next few hours and note any changes to share with your healthcare team.
When to Call Your Doctor or 911
Deciding when to manage symptoms at home, call your doctor, or seek emergency care can be tricky. Use the table below to guide your decisions:
| Situation | Symptoms | Action | Timeframe |
|---|---|---|---|
| Manage at Home | Mild shortness of breath, slight cough changes, relief with rescue inhaler | Follow your action plan, rest, and monitor | Monitor for 24–48 hours |
| Call Your Doctor | Frequent use of rescue inhaler (more than every 4 hours), persistent fatigue, sputum changes, low-grade fever (99–101°F) | Contact your doctor the same day | Within 2–4 hours of symptom onset |
| Call 911 Immediately | Severe breathing difficulty, chest pain, confusion, blue lips or fingernails, oxygen levels below 85% | Seek emergency care immediately | Call right away |
If your symptoms don’t improve after using your rescue inhaler, or if you notice troubling changes - like persistent fatigue, unusual sputum color, or needing your inhaler more often than usual - contact your doctor promptly. These changes could indicate an infection or other complications.
Call 911 without delay if you experience severe breathing trouble that doesn’t improve with your inhaler, chest pain, confusion, or blue/gray lips or fingernails. These are signs that your oxygen levels are dangerously low and require immediate medical attention.
Your familiarity with your own symptoms is key. If something feels significantly different or alarming, even if it doesn’t fit neatly into these categories, trust your instincts and seek medical advice. It’s always better to err on the side of caution.
When reaching out for help, have your medication list, recent symptom changes, and vital signs (if available) ready to share. This information helps medical professionals assess your situation quickly and provide the right care.
How to Prevent Future Exacerbations
Preventing COPD exacerbations is just as important as treating them when they happen. According to Dr. Uddalak Majumdar, a pulmonologist: "Preventing exacerbations is an essential part of treatment" and "Each flare-up can cause small but permanent lung damage" [11]. Taking deliberate steps to limit triggers and stick to your treatment plan can greatly lower the chances of future episodes.
Avoid Common Triggers
One of the best ways to prevent flare-ups is by identifying and avoiding the things that trigger your symptoms. Environmental factors are often the main culprits, and many of these can be managed with the right precautions.
Smoke exposure is a major trigger. This includes cigarette smoke, secondhand smoke, and even wood fires [1][11]. If you smoke, quitting is essential. Avoid areas where smoking occurs, as secondhand smoke can also worsen symptoms.
Strong scents and chemicals can irritate your airways. Opt for unscented personal care products and cleaning supplies [1][11]. Avoid scented candles, air fresheners, and use cleaning products in well-ventilated spaces.
Air quality is another critical factor. Check daily pollen counts and air quality index (AQI) reports, and adjust your outdoor activities accordingly [1]. On days with poor air quality or high pollen levels, stay indoors or limit outdoor activities to early morning or evening when conditions are better.
Weather changes can also affect your breathing. Cold air, wind, sudden temperature shifts, and high humidity are all potential triggers [1][11][12]. On cold or windy days, use a scarf loosely wrapped around your face to protect your airways [1][12]. On hot or humid days, air conditioning can help maintain a comfortable indoor environment [1].
Maintain indoor humidity at about 40% using a humidifier [1][12]. This can prevent your airways from drying out. Air purifiers can also help by removing dust, allergens, and other particles from your home. For those exposed to occupational hazards, consult your doctor about reducing exposure [1].
By controlling your environment and avoiding triggers, you can work alongside your treatment plan to minimize the risk of exacerbations.
Stay Consistent with Treatment
Avoiding triggers is just one part of the equation - sticking to your treatment plan is equally important. Consistent use of prescribed medications can help keep exacerbations at bay. This means taking your medications as directed, even on days when you feel fine.
Medication adherence is crucial [13]. Long-term control medications and oxygen therapy (if prescribed) need to be taken regularly to maintain steady levels in your system. Even during "green zone" days when symptoms are minimal, continuing your treatment is essential.
It’s helpful to understand your medications. Know the names, dosages, and schedules for everything you take, including inhalers (short-acting, long-acting, and steroid types) and tablets like theophylline, mucolytics, or antibiotics [13][14]. If you’re unsure about your inhaler technique, ask your doctor or nurse for guidance to ensure the medication reaches your lungs effectively [14].
Monitoring your condition daily can help you catch problems early. Keep track of your COPD symptoms, sleep patterns, and overall well-being [13]. This information can help identify changes before they escalate. Some medications, like theophylline, may require regular blood tests to ensure the dosage is right while minimizing side effects [14].
Preventive healthcare is also key. Stay up to date on vaccinations, especially annual flu shots and pneumonia vaccines, as respiratory infections can trigger exacerbations. Have emergency medications, such as steroid tablets or antibiotics, on hand to use at the first sign of a flare-up [13].
Regular check-ups with your healthcare provider are essential. These visits allow for adjustments to your treatment plan, reviews of inhaler techniques, and early detection of any changes in your condition.
Educational and Support Resources from COPD Essentials
In addition to managing triggers and sticking to your treatment plan, staying informed and proactive can further improve your COPD management. COPD Essentials offers a range of resources tailored to help individuals living with COPD.
The platform provides educational articles and guides that explain COPD management strategies, treatment options, and lifestyle changes in a clear, actionable way. These resources are designed to help you implement practical advice in your daily life.
COPD Essentials also offers tools to help you monitor your condition. These include pulse oximeters to track oxygen levels, home spirometers to monitor lung function, and peak flow meters to assess breathing capacity. These devices can alert you to changes in your condition and provide useful data for discussions with your healthcare team.
For your home environment, the site features air quality monitors, HEPA air purifiers to reduce allergens and pollutants, and humidifiers or dehumidifiers to maintain optimal humidity levels. These tools can help create a safer and more comfortable living space.
Digital health tools are another valuable resource. COPD Essentials highlights apps for symptom tracking, medication reminders, and overall COPD management. Many of these apps generate reports, making it easier to share updates with your healthcare provider.
Finally, the platform offers support for both patients and caregivers. This includes caregiver guides, information on support groups, and educational courses to help you and your loved ones better understand and manage COPD. By taking advantage of these resources, you can stay informed, organized, and proactive in preventing future exacerbations.
All products and resources on COPD Essentials are carefully selected by health researchers, ensuring they provide practical tools and information to enhance your quality of life.
Conclusion: Take Control of Your COPD Management
Using early detection strategies as a foundation, consistent monitoring and preparation can help you address problems before they grow into larger issues. Keep track of your oxygen levels with a pulse oximeter, jot down daily symptoms in a diary, and stick to your COPD action plan to stay on top of your condition.
You know your body best. Pay attention to changes - like a cough that feels unusual, increased breathlessness while climbing stairs, or more difficulty completing everyday tasks. These small observations, when paired with your action plan, can guide you in managing your care effectively.
COPD Essentials offers tools and resources designed to support your efforts. From pulse oximeters and home spirometers to symptom tracking tools, these devices can help you spot trends and communicate clearly with your healthcare team.
Managing COPD isn’t about doing it all on your own - it’s about staying informed, prepared, and working closely with your care providers. With the right knowledge, tools, and support, you can reduce the risk of flare-ups and maintain your quality of life. Each step you take toward prevention and early detection is a step toward protecting your health and independence.
FAQs
When managed properly, COPD symptoms like a persistent cough, mucus production, shortness of breath, wheezing, chest tightness, and fatigue usually stay consistent. But a COPD exacerbation can cause these symptoms to suddenly get worse. Some warning signs to watch for include:
- A noticeable increase in coughing or frequency
- Mucus that changes in color, thickness, or quantity
- Shortness of breath that becomes more intense and doesn’t improve with your usual treatments
If these changes persist for two or more days, it could signal an exacerbation. Prompt action is crucial - contact your healthcare provider and follow your COPD Action Plan. Addressing the issue early can help stabilize your symptoms and reduce the risk of further complications.
If you notice signs of a COPD flare-up - like more frequent coughing, worsening shortness of breath, changes in mucus (such as its color, thickness, or amount), wheezing, or a feeling of chest tightness - it's important to act quickly. Start by using your prescribed rescue inhaler and follow the treatment plan your doctor has provided. If you use supplemental oxygen, only adjust the levels as directed by your healthcare provider.
Some symptoms require immediate emergency care. These include severe trouble breathing, confusion, unusual drowsiness, chest pain, or symptoms that rapidly worsen even after using your usual treatments. These could signal a life-threatening situation, so don’t hesitate - call 911 right away. Quick action can make all the difference in effectively managing a COPD exacerbation.
Preventing COPD flare-ups during seasonal shifts or on high-pollution days starts with limiting outdoor exposure when air quality takes a hit. Indoors, consider using an air purifier to cut down on allergens and irritants, and aim to maintain humidity levels between 30–50% to keep your airways comfortable. Staying hydrated and avoiding triggers like exhaust fumes or heavily scented products can also make a big difference.
It's also smart to monitor weather and air quality updates, especially during seasonal transitions, so you can adjust your plans accordingly. These small but effective steps can help lower the chances of exacerbations and make it easier to breathe no matter the time of year.
